My Story:
Zack
From Hawkes Bay
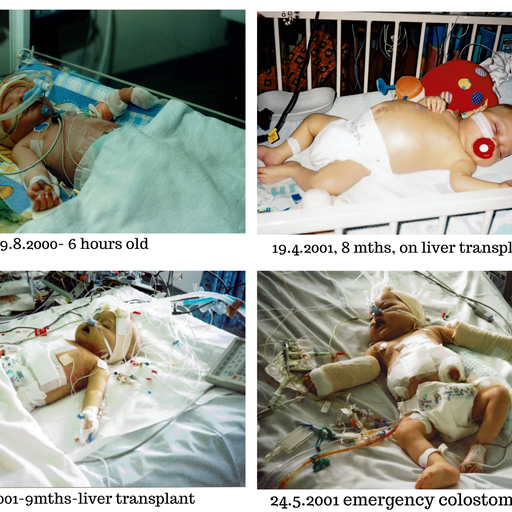
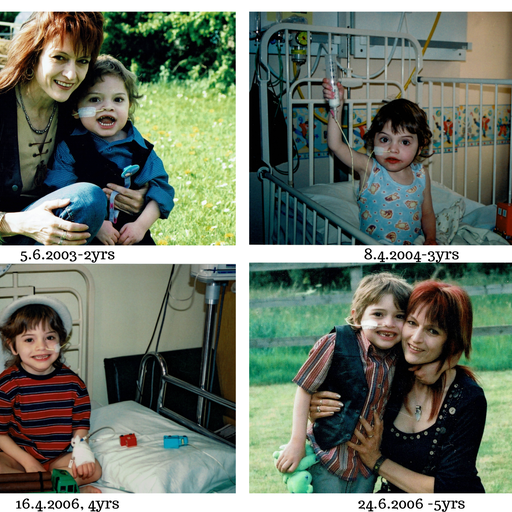
Zack – only child, born 9th August 2000, 38 weeks, 6lbs 6oz
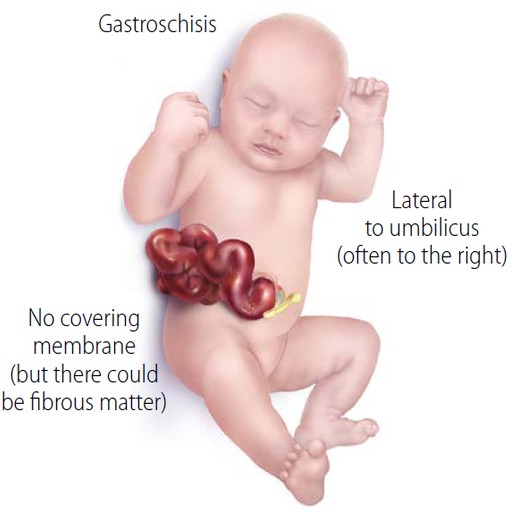
Zack was born with Gastroschisis –– a birth defect of the abdominal wall resulting in the baby’s intestines slipping through a hole near the belly button.
Detected on my 12 week scan, Zack’s case was particularly severe – his entire small bowel (where most of the digestive process takes place), was floating in amniotic fluid.
His birth-date was unexpectedly brought forward due to the rapidly deteriorating intestine and he was born at 38 weeks with septicaemia which further hindered his chance of survival. Zack was transferred immediately to Sheffield Children’s Hospital where the necrotic sections of small bowel were removed and the remainder of his intestines returned to the abdominal cavity in the hope they may eventually function. He only had a third of his small bowel left and unfortunately this was badly damaged.
Life-threatening complications followed over the months due to the non-functioning bowel and numerous infections. Further operations on the bowel ensued, all of which carried huge risks due to Zack’s fragility.
Unable to be fed orally due to the poor condition of his bowel, Zack was sustained by TPN (Total Parenteral Nutrition) which gave him the essential nutrients he needed via a central line, pumping them straight into his bloodstream. This in turn, put Zack at risk of line infection, of which there were many, thus needing several trips to theatre for line replacement and IV antibiotics.
Zack was now 6 months old and as of yet had not been home.
Devastatingly, due to Zack’s poor metabolic state and the artificial method of feeding, the TPN damaged his liver and at 7 months old he suddenly went into irreversible liver failure. He was transferred as an emergency at 2am to Birmingham Children’s Hospital Liver Unit where he was listed immediately for a liver and bowel transplant. Miles from home, I was given a room at the Ronald McDonald accommodation close to the hospital. This was to become my home for nearly two years.
The seriousness of the situation hit me like a ton of bricks. Despite being a nurse, I had never dealt with this field at all and the fact it was my child this was happening to was extremely difficult to come to terms with. I put all my faith in Zack’s medical and surgical teams, knowing they would do their very best for him.
Finding a suitable donor was greatly hindered as Zack was unable to receive a portion of an adult’s liver – he needed a whole liver with an intact bile duct to connect it successfully to the bowel. Usually a bile duct is fashioned from the intestine but Zack hadn’t enough intestines left in order to do this. This meant Zack had to have a baby’s liver which were extremely scarce. Finding a donor bowel was even more difficult as this organ was not commonly donated. The surgeons knew time was running out and decided to do an isolated liver transplant should one become available, to buy Zack time whilst the search for a small bowel continued.
Zack became increasingly more jaundiced, swollen and weaker as his body was unable to cope with the build-up of toxins. After a fraught 6 week wait during which Zack was heart-stoppingly temporarily taken off the list due to a high temperature, a baby’s liver thankfully became available and he underwent his 16 hour life-saving transplant. This was a bittersweet moment for me. Obviously I was immensely relieved and grateful that Zack was being given this amazing opportunity, but at the same time I was terribly upset for the poor mother who had just lost her child. It took years for the guilt to leave me even though I knew she had wanted to donate her child’s organs so her child’s death would not have been in vain.
During Zack’s transplant, his surgeon examined the small section of intestine Zack had left and felt he could salvage it, thus avoiding a bowel transplant. This was great news as back in 2001, a bowel transplant was a relatively new procedure and carried a high mortality rate. I was so relieved to hear Zack may not require one after all. The bowel transplant programme has improved significantly over the years and now has a much higher success rate.
I was warned that Zack would remain in hospital for the unforeseeable future as it would take a long time for his damaged bowel to adapt and the path he was going down was fraught with potential life-threatening complications. He would need constant IV support and close monitoring. It was also unlikely that Zack would ever eat normally. None of this mattered to me, as long as he could avoid a bowel transplant…
Zack also had his appendix removed during his transplant as it was discovered to be on the wrong side of his body. This would avoid any confusion in the future should he have suspected appendicitis. My baby boy was not only “inside out”, but “back to front” as well!
Complications soon hit Zack post-transplant. In ICU – each lung collapsed within days of each other, he developed a chest infection, a bowel infection, and renal problems. His bowel perforated twice, resulting in an emergency jejunostomy and a stoma bag. He also had great difficulty being weaned off the ventilator. Zack’s expected 72 hours in ICU became 3 weeks!
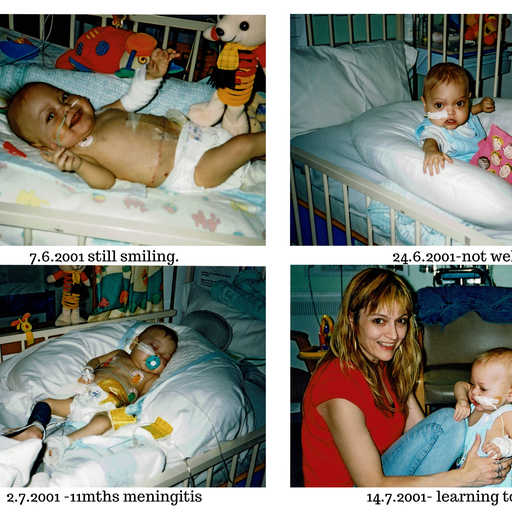
Zack finally went back to the Liver Unit’s High Dependency Unit where he unfortunately contracted meningitis and went into major liver rejection. He was a very poorly boy!
The organ rejection was a mystery at first. A transit time test was performed by putting red dye down his NG tube. It was expected that the dye would appear in Zack’s stoma bag in approximately 4 hours – it arrived in 12 MINUTES! This meant his anti-rejection medication was shooting through his digestive system straight into his stoma bag, not having time to be absorbed. Although he was meant to have the stoma for at least a couple of years to rest the damaged bowel, he was taken straight to theatre for an emergency stoma reversal to increase the absorption capacity. He was also given his anti-rejection drug through an IV which was an unusual but necessary procedure. After three days this had to be discontinued as it was causing severe damage to his veins. It was successful though and got him out of trouble. Recurring line and bowel infections continued and Zack had yet another bowel operation after contracting necrotising enterocolitis which caused further damage to his gut. His rapid weight loss during this time was frightening. It really was one step forward and two steps back!
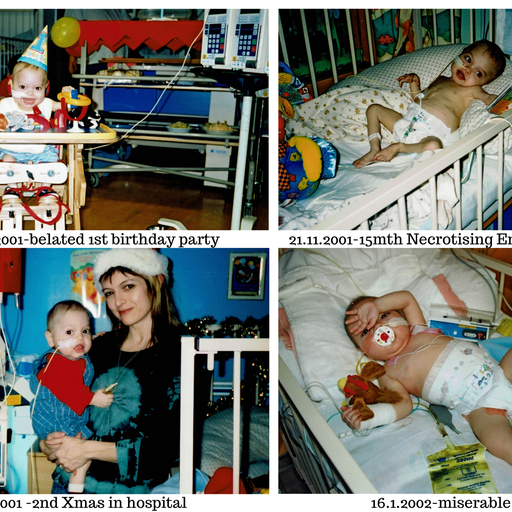
With Zack’s small bowel and suppressed immune system continually causing major set-backs, home was still not an option and in January 2002 (now aged 1 year, 5 months), Zack underwent a procedure known as a “Bianchi,” named after the surgeon Mr Bianchi who developed this technique of bowel lengthening. Zack, I believe, was only the second child in Birmingham Children’s Hospital to undergo this technique. Unfortunately, after the 8 hour op, due to Zack’s bowel being too short to work with, it wasn’t successful but his surgeon, Mr De Ville, was able to improve the distended sections of Zack’s bowel significantly, thus making a huge change to the overall outcome. It meant Zack would eventually be free of TPN and could survive on tube-feeding alone. It would take further months in hospital for the bowel to adapt but the wait would be well worth it.
After spending his first Christmas, first birthday and second Christmas in hospital, Zack finally came home for the first time Feb 2002 – a walking toddler!
Devastatingly, his father walked out on us which came as a huge shock. He also chose not to be a part of Zack’s life. My immediate family all resided in New Zealand but it was out of the question for Zack to move there – his health was too unstable and he needed the ongoing care of his UK doctors.
Zack came home attached to a 24 hour feeding pump via his naso-gastric tube – difficult for a little boy nearly 2 years old, excited to explore a whole new world that was now available to him. By age 4 years he was able to have 4 hours a day off his pump. We made good use of this “freedom” – going to the park, running in fields etc. and finally attending pre-school with a carer in tow.
Initially he could only have one visitor to the house at a time and they had to wear masks, sterilise their hands etc due to Zack’s low immunity.
Due to Zack being dependent on naso-gastric feeding thus not chewing, his speech muscles which are closely linked had not developed and Zack was unable to verbally communicate. This caused him great frustration so I learnt basic Makaton (sign language aimed for children). Zack was quick to pick it up and the realisation that he could ask me for a drink of water or tell me if he was tired was such a delight for us both. The first words he learnt in Makaton by the way, were ‘please’ and ‘thank you’! Intensive speech lessons later helped and by age 6 one would never have known there had been such a delay.
Zack had a special liver feed that I made up each day. This consisted of mixing together several different powders and liquids. It would take me well up to half an hour with all his medications as well and heaven help me should I be distracted half-way through, I would lose my place and have to start all over again!
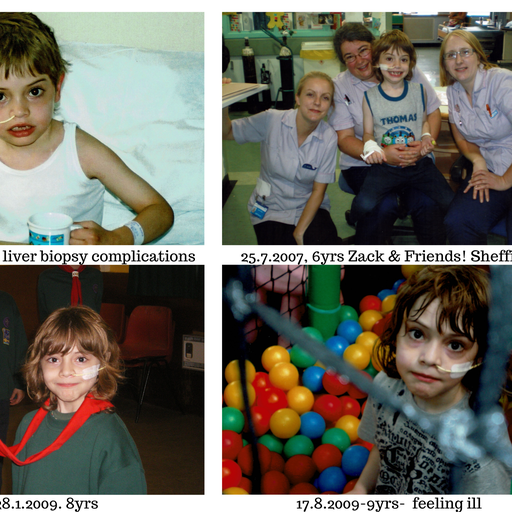
Unfortunately, due to the fragile state of Zack’s short bowel and his suppressed immune system, Zack had many hospital admissions over the following years – most of them being via emergency ambulances as he would fall seriously ill extremely quickly and without warning.
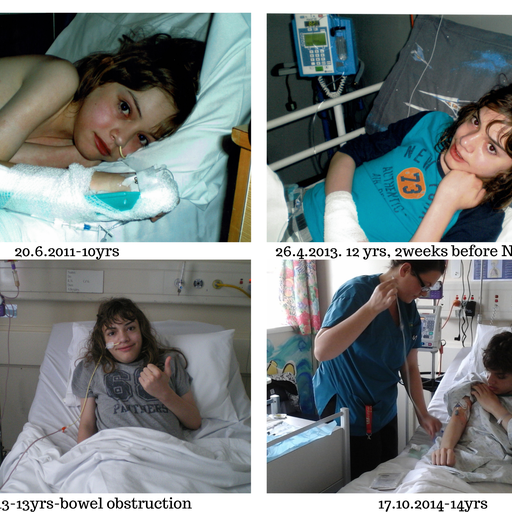
He would be running around one minute, then vomiting severely the next. Unexplained rashes would appear- one in particular when he was 10 being so severe he was hospitalised for nearly 2 weeks, tested for 81 viruses but still it remained a mystery! His hospital stays were long as each incident would result in complications. Zack began to regard Sheffield Children’s Hospital as his second home which was a blessing as it reduced the fear somewhat for him.
At age 10, Zack became increasingly concerned that should something happen to me, there was no one to take care of him. It made sense to take him to New Zealand to be with his Grandma, Grandad, Aunty, Uncle and cousins. At age 12 he was finally deemed fit enough to endure the long flight to NZ. It was most reassuring to know that Dr Helen Evans at Auckland’s Starship Hospital would be in charge of Zack’s care upon our arrival as amazingly, Helen had been one of Zack’s liver transplant doctors in Birmingham!
In New Zealand, Zack’s problematic bowel and suppressed immune system continued to result in many admissions to Starship and our local Hawkes Bay Hospital where he was under the care of Dr Jenny Corban.
Costochondritis (inflammation of the cartilage which attaches the ribs to the sternum – as painful as a heart attack), dermatographia (hyper-sensitive skin) so extreme that Zack would need to be sedated for any external procedures such as blood taking, H.pylori (infection in the bowel), oesinophilic oesophagitis (allergy cells in the oesophagus), cholangitis, (inflammation of the bile duct), bile duct stricture, (theatre again) were some of the conditions he suffered.
At age 14, Zack developed chronic pain syndrome which affected him terribly. Walking became increasingly difficult. He was unable to socialise and spent many hours in bed as he couldn’t tolerate a sitting position due to the pain in his stomach. Rashes and welts became a daily occurrence. We were flown back to Starship to see an immunologist and surprisingly, Jon Bishop, a gastroenterologist at Starship who knew Zack from Sheffield Children’s Hospital!
Zack’s whole immune system had gone haywire. Several medications were tried over the next few months but nothing was helping. He was left with permanent Raynaud’s syndrome (blood circulatory problem affecting the extremities), - the result of a rare side-effect of a medication tried in an attempt to tone down the severity of his chronic pain.
Zack could no longer attend mainstream school due to his long absences. This devastated him as he enjoyed the social interaction.
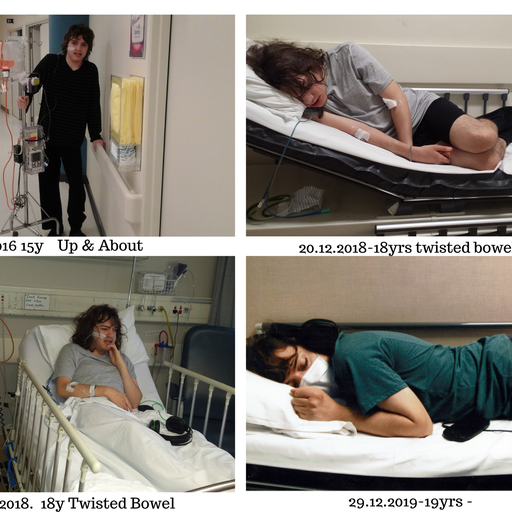
At age 15, Zack was unable to cope any longer and had a complete and utter meltdown. He was admitted to hospital for assessment, put forward for counselling and was prescribed further off-label medication to help combat the pain.
Unfortunately Zack again was affected by a rare reaction to one of his painkillers. He experienced acute episodes of confusion and memory loss and has since been diagnosed with Functional Neurological Disorder. This diagnosis was a relief for Zack as he was becoming increasingly frightened with his episodes of “fogginess” and feared he was losing his mind!
His symptoms are less severe now although remain problematic at times.
Back to Starship again where a camera capsule was put down Zack’s oesophagus to track along his digestive system, taking hundreds of photos as it went along. This should have been passed out naturally in 24 hours but it got stuck in a distended bowel loop. 30 days later, after countless X-rays and many failed attempts to extract the capsule, Zack was discharged home to wait for a date for surgical intervention.
After two emergency blood transfusions due to an internal bleed at home, Zack went back to Starship for another 6 week stay. He underwent an 8 hour operation to remove the camera capsule found floating up and down in his distended bowel. Much to the surgeon’s surprise, he also came across a Lego SpongeBob Squarepants Krabby Patty (burger) which Zack had swallowed when he was 8 years old – now twice its normal size, calcified and fossilised after floating around in the same section of non-functioning bowel for 8 years! Zack was given it as a keepsake!
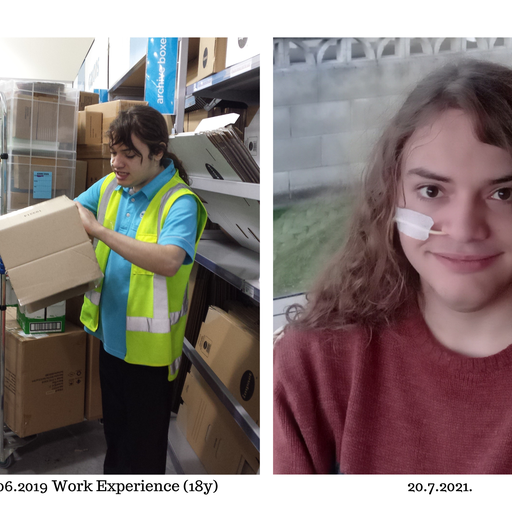
The operation took so long due to the excessive amount of adhesions and scar tissue “gluing” the intestine together hindering access. His surgeon, Stephen Evans, “tidied” the loops of dilated bowel (the worst he had ever seen!), thus greatly improving bowel function and at age 17, Zack FINALLY came off his overnight feed pump, able to get by on drinking the formula in the daytime.
He is actually able to eat a small variety of food and this year, aged 20, finally came off his formula altogether! He still has his NG tube for meds and hydration emergencies which is fine.
Zack has 4 weekly blood tests to ensure the liver is functioning satisfactorily and five yearly liver biopsies. A plethora of medicines including anti-rejection drugs are taken via his NG tube twice a day. He still suffers vomiting bouts, has been back in hospital with a twisted bowel and has several “off” days. However, his chronic pain is much reduced and Zack is able to lead a much more normal life.
Zack turned 21 in August - an age he was never expected to reach.
He is planning on taking a computer course at college next year (Covid permitting) and to gain his Learner Driving Licence.
Despite all he has been through, Zack remains unbelievably cheerful and stoic. He appreciates the second chance of life he was given and has faced adversity with immense bravery/courage. He has never complained, nor asked, “Why me?”
We are both so very thankful for all the medical and surgical help he has received over the years from Sheffield Children’s Hospital, Birmingham Children’s Hospital Liver Unit, Starship Hospital, and Hawkes Bay Hospital.
We have been informed that Zack will require a second liver transplant before he’s 30! Zack and I will face it head on…..
Written by Lucinda Gay, (Mum).